Case Study: Fixing Thoracic Outlet Syndrome
December 10, 2021 | Functional Range Conditioning

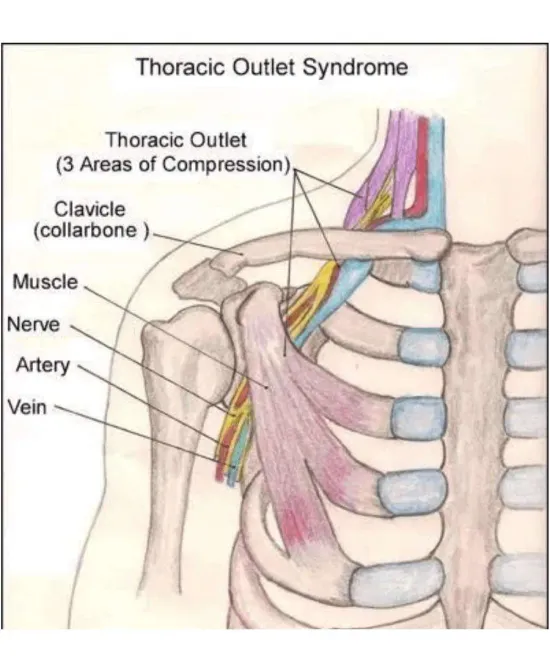
Thoracic outlet syndrome (TOS) is a blanket term for compression of the first rib and collarbone. It often results in nerve pain, discomfort, and numbness in the arm or extremities.
Unfortunately, the cause of thoracic outlet syndrome is unclear. However, we know genetics play a role, as can traumas or lifestyle-related activities.
Anyone with TOS will tell you that it’s an unpleasant, life-altering syndrome. It is debilitating and painful and a general deterrent from activities that require you to use your arm.
Prognoses for TOS are often gloomy, resulting in people feeling like they have to live with the outcome of their condition. Further, someone with thoracic outlet syndrome will usually hear that no effective treatment exists aside from surgery.
Our approach at Motive Training offers a unique ray of hope in this situation, providing a fresh perspective on TOS treatment.
Meet Kira, a hard-working mother of one who was long ago diagnosed with thoracic outlet syndrome on her right side. As a result of her condition, she experienced pain and discomfort in her neck and shoulder, which progressed down to the elbow. So, in essence, Kira’s right arm wasn’t working very well.
But before we get to Kira’s story, let’s dive deeper into thoracic outlet syndrome.
What is Thoracic Outlet Syndrome?
Definition And Overview
Thoracic outlet syndrome is a collection of disorders that arise when the nerves and/or blood vessels in the thoracic outlet are compressed. The thoracic outlet is the narrow space between your collarbone (clavicle) and your first rib. This area is crucial because it houses the nerves and blood vessels that supply your shoulder and arm. When these structures are squeezed or compressed, it can lead to various symptoms, including pain, numbness, and weakness in the upper extremities. Understanding thoracic outlet syndrome is the first step in recognizing and addressing the discomfort it can cause.
Symptoms And Causes
Common Symptoms Of Thoracic Outlet Syndrome
The symptoms of thoracic outlet syndrome can differ based on which structures—nerves or blood vessels—are being compressed. Here are some common signs to watch out for:
-
Pain Or Numbness: You might feel pain or numbness in your neck, shoulder, or arm.
-
Weakness Or Fatigue: Your arm or hand may feel weak or tire easily.
-
Tingling Or Burning Sensations: These uncomfortable sensations can occur in your arm or hand.
-
Coldness Or Discoloration: Your arm or hand might feel cold or appear discolored.
-
Swelling Or Redness: You could notice swelling or redness in your arm or hand.
Recognizing and addressing these symptoms early is crucial, as it can significantly impact your daily life and empower you to take control of your health.
It’s important to note that diagnosing thoracic outlet syndrome is best done by a doctor and physical therapist. Once you have the correct diagnosis, we at Motive Training can help you work with it.
Risk Factors And Contributing Conditions
Several factors can increase your risk of developing thoracic outlet syndrome. Here are some key contributors:
-
Congenital Factors: Some people are born with a narrow thoracic outlet or an extra rib, known as a cervical rib, which can predispose them to thoracic outlet syndrome.
-
Trauma: Sudden injuries or chronic overuse can lead to the development of TOS.
-
Poor Posture Or Muscle Imbalances: Slouching or having imbalanced muscles can contribute to compression in the thoracic outlet.
-
Repetitive Strain: Activities involving repetitive shoulder and arm use, such as certain sports or occupations, can increase the risk.
-
Other Conditions: Tumors or cysts in the thoracic outlet can also cause compression.
Recognizing these risk factors can empower you to take preventive measures and seek early treatment, putting you in control of your health.
As We Always Say: Assess, Don’t Guess
Back to Kira.
When she stepped foot into Motive Training, we first took baseline videos of her doing shoulder CARs (click here to learn what CARs are) using the Functional Range Assessment (FRA). We use the FRA to examine how joints move independently, which you can learn more about here.
Diagnosing thoracic outlet syndrome requires a comprehensive process, including a physical examination, client history, and various imaging tests to identify the condition accurately. Imaging is generally done by a specialist, not us at Motive Training. Sometimes, it is not required, as a physical therapist can often diagnose the condition without imaging.
In any case, we noticed Kira couldn’t bring her arm overhead. The picture shows her limited active shoulder flexion. Given her condition, a slight degree of elbow bend is somewhat normal, but this is where her shoulder flexion capped out.
You can’t see that Kira also compensated heavily through her neck and lumbar spine to attempt to get more out of her shoulder. We see this often in someone who lacks overhead shoulder mobility.

So, not only was Kira not able to use her shoulder, but she was also more likely to use her back, neck, or elbow every time she went to use her shoulder.
You’re Not Stuck, But You Have Been Led To Believe That
Many people in Kira’s situation feel like they’re in a similar boat, unable to improve their situation. We understand this struggle and are here to provide support and effective solutions.
”Make Sure To Stretch.”
Yeah, okay. How long? How often? What are you supposed to stretch? What’s the best way to do so? What are you trying to feel?
A physical therapist can guide you through effective stretching exercises and provide professional supervision for personalized exercise programs tailored to your condition. However, their methods are generally antiquated and underperformed; this is a bold claim, but if you saw the number of people coming to Motive Training post-rehab, you’d know why we feel this way.
”Move Your Body, But Cautiously With Physical Therapy.”
So, do things that don’t hurt but avoid things that might hurt, which could include anything and everything. Great.
Movement is crucial for improving posture and strengthening muscles that impact thoracic outlet syndrome. You don’t need to do it with a physical therapist, but it can be effectively combined with other treatments, like manual therapy and massage, for comprehensive management of TOS.
Or Better Yet, “Rest.”
Continue not moving, so the thing that hurts when you move it hurts because you tried to inevitably move it—got it.
The truth is that most movement conditions can be helped (not fixed) by directing effort in the right places, at the correct times, and for long periods. This is precisely what we do in the gym.
Functional Range Conditioning (FRC) Can Change Your Life
We used principles from Functional Range Conditioning (FRC) and more directly attacked Kira’s shoulder. We worked on internal rotation and flexion, doing PAILs/RAILs (as seen below), passive range holds, lift-offs, etc. Early treatment to treat thoracic outlet syndrome is crucial to prevent serious complications such as increased pain and blood clots.
Simply put, we showed her what her shoulder was missing regarding movement. Then, we taught her how to correctly engage stretches and hold positions for better outcomes. We expressed the importance of doing all of this continuously (the more inputs, the better!).
In this new picture (5 months later), you see a drastic difference in Kira’s ability to move her shoulder.
Not only is this an incredible jump in range of motion, but her pain went down, her neck stiffness decreased, and she doesn’t ever mention her elbow pain.
This is why we do what we do!

Thoracic Outlet Syndrome Is Treatable
As Dr. Spina from FRC says, if you try to do shoulder stuff with a shoulder that doesn’t work, you’re probably not doing shoulder stuff but shoulder compensation stuff. Our goal is to show you how to actually move your body in a way that leads to real, sustainable change.
For those suffering from neurogenic thoracic outlet syndrome, venous thoracic outlet syndrome (sometimes referred to as vascular thoracic outlet syndrome), or general thoracic outlet syndrome, corrective exercise, mobility and stretching methods from FRC, and manual inputs (e.g., Functional Release) can help alleviate symptoms associated with nerve compression in the thoracic outlet. So, if you’re stuck like Kira was, reach out, and we’ll show you a better way.
You don’t have to be beholden to your doctor’s prognosis. However, thoracic outlet syndrome treatment can vary based on whether the syndrome is classified as neurogenic or vascular. So, it is ultimately crucial that you speak with your doctor or physical therapist if you are dealing with this condition.
There is hope, though, and we’re here to help.
Written by
Brian Murray, FRA, FRSC
Founder of Motive Training
We’ll teach you how to move with purpose so you can lead a healthy, strong, and pain-free life. Our headquarters are in Austin, TX, but you can work with us online by signing up for KINSTRETCH Online or digging deep into one of our Motive Mobility Blueprints.

